- Important, Not Important
- Posts
- 🧠 Explainer: Antimicrobial Resistance
🧠 Explainer: Antimicrobial Resistance
A 101 on antimicrobial resistance

What is antimicrobial resistance?
Antimicrobials are medicines that we use to prevent and treat infectious diseases caused by pathogens like bacteria, viruses, fungi, and parasites.
Chances are you are most familiar with antibiotics, but antiviral, antifungal, and anti-parasitics all exist too, and are all at risk of developing resistance. How fun!
We’ve been locked in an evolutionary arms race with these tiny organisms since the dawn of time, but in the 20th century the discovery of antibiotics in particular, like penicillin, caused human life expectancy to skyrocket from around 47 years to 78.
Take that, diphtheria!
But, organisms like bacteria and viruses have been around a lot longer than we have, and they’re pretty good at the whole survival of the fittest thing.
And while we’ve been focused on things like finding exponentially more outrageous toppings for poutine, pathogens have been reproducing exponentially and developing a resistance to antimicrobial medicines — and this time, the Resistance are the bad guys (if you happen to be human, that is).
What are the main causes of antimicrobial resistance?
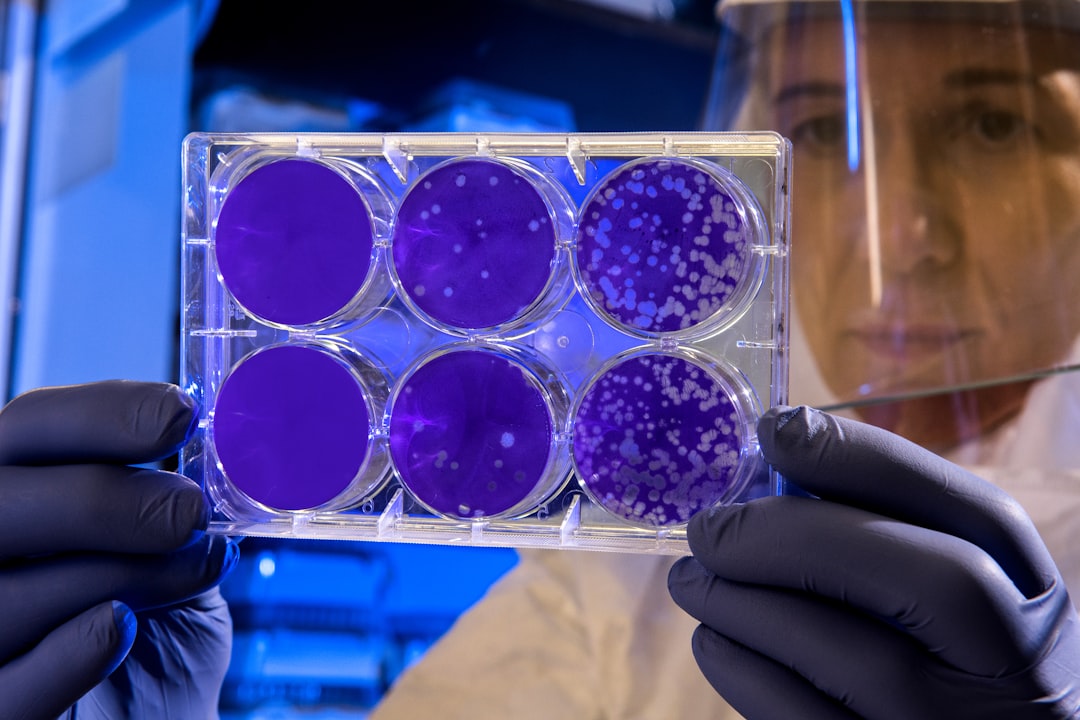
Pathogens develop resistance over time due to natural processes like selective pressure, mutation, and gene transfer.
Some individuals will have a mutation or natural resistance to medicine, meaning that if the rest of the population is wiped out, the only gene pool that remains is the one that has those resistive qualities, and the speed at which pathogens reproduce means that soon the entire strain is now resistant to that medicine.
When we use antimicrobials inappropriately, we amp up that selective pressure.
When we prescribe antibiotics to treat a viral infection or use a broad-spectrum antibiotic where a specific one would have been better, or if we don’t complete a full treatment of medicine, resistance spreads.
It also tends to spread in hospitals, where sick people are more likely to get an infection.
Antimicrobial medicines are the foundation of modern medicine, and the spread of resistant pathogens is a huge threat to our ability to perform medicine, from common ailments like UTIs to procedures that save lives, like chemotherapy.
The 2022 Global Antimicrobial Resistance and Use Surveillance System report found that one in five cases of UTIs caused by E. coli were resistant to standard antibiotics in 76 countries.
Almost 5 million people died due to AMR in 2019 (mostly in sub-Saharan Africa, where drug resistance to malaria and TB is a concern).
Just 6 pathogens are responsible for over 75% of bacterial AMR deaths. This could increase to 10 million per year by 2050, and become the leading cause of death worldwide.

Antimicrobials in food
And we don’t just use antimicrobials in health care. Over half of antibiotics produced in the US are used in agriculture.
We rely on them in our agricultural systems to treat animals and plants, which means in addition to potentially causing havoc in our healthcare systems, antimicrobial resistance poses a huge threat to food security.
Antimicrobial resistance that develops in humans and livestock can spread to waterways and soils, via human and animal waste, especially in places without adequate sanitation systems.
We use them on our crops too, which can also have detrimental effects on the surrounding environment, as pesticide use can spread to surrounding soil and water.
And we don’t just use the on land either. The use of antimicrobials in aquaculture contaminates the local aquatic environment, and pathogens can easily spread from farmed fish to wild populations.
AMR national action plans
Given the seriousness of AMR as a threat to our health care and food systems, two things that are hanging on by a thread as it is, countries are taking action.
At the 2015 World Health Assembly, countries adopted the Global Action Plan on AMR, which has also led to the AMR Multi-Partner Trust Fund.
Since then, 178 countries have developed national action plans that align with the GAP. These action plans include, but aren’t limited to:
Ensuring global access to safe, clean drinking water
Improving AMR surveillance and global public health collaboration
Increasing public education on the risks and proper uses of antimicrobials
You can check to see how your country is doing on implementing AMR action plans here.
How do you fix antimicrobial resistance?
Like most problems, there’s no silver bullet solution to AMR.
Other than continuing to fund research to develop new, more effective antimicrobials, the best solution is prevention.
Germs are spread from person to person via contact with contaminated hands, surfaces, and equipment. So, in case you haven’t learned anything since 2020, WASH YOUR HANDS. Even if you don’t work in a hospital. Just do it, ok? Please? Don’t be gross.
Other ways to prevent AMR:
Avoid over-prescribing of antibiotics. Antibiotics do not work against viruses. Say that into the mirror five times every day until it sticks.
If you do need antibiotics because you have a bacterial infection, complete the entire course of the prescription so that it can be fully effective and not breed resistance.
Get vaccinated (again, things we should have learned since 2020)
Eat less meat and other animal byproducts, especially from animals farmed by industrial agriculture
Buy local, organic produce where you can
Reply